Understanding Fistulas and Treatment Options
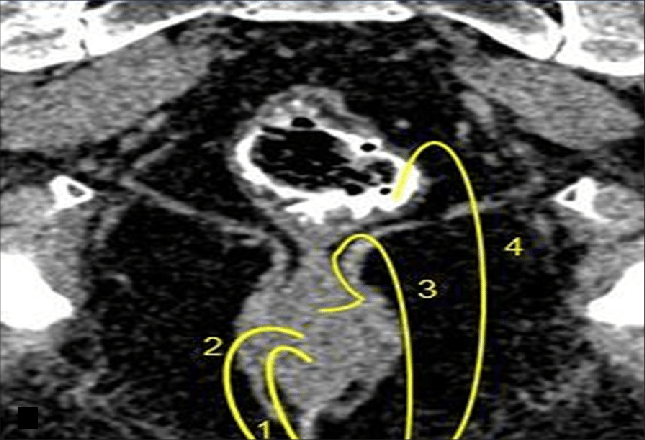
Fistulas can be a challenging and complex part of living with Perianal Crohn’s disease. As you’ll see in the charts provided, there are several types of fistulas, each requiring a unique approach to treatment. It’s not uncommon to have multiple fistulas at once, and they can often branch out like tree roots, leading to what are known as complex fistulas—particularly if they involve a significant portion of the sphincter muscle.
On the following pages, you’ll find detailed information about various treatment options, including setons (small rubber band-like sutures looped through the fistula), fistulotomies, FiLaC, biologics, and antibiotic therapy. It’s important to approach treatment cautiously—research has shown that certain procedures, like placing setons during the initial abscess, can sometimes cause more harm than good.
Before making any decisions about treatment options, such as corrective surgeries, colon diversion surgery (ostomy), or a proctectomy, I strongly encourage you to seek second opinions and explore every avenue. While some surgeons report high success rates for these procedures, data shows that only 18% to 33% of people achieve remission. For others, complications or worsening conditions may occur.
This website is a growing resource. I’m continually adding new content, so be sure to check back often. If you have questions, suggestions, or need support, please don’t hesitate to reach out to me at fistulizingcrohns@gmail.com. I’d also be honored to share your story on my blog to inspire and connect with others navigating this journey.
Fistula Treatments
Fistulas associated with Crohn’s disease can vary in complexity, and their management requires a tailored approach based on the type, severity, and patient’s overall health. Below, we detail the different types of fistulas and the corresponding treatment options.
Submucosal Superficial Fistulas (with or without Abscess)
These fistulas are the least complex and involve minimal or no involvement of the anal sphincter. Treatment options include:
- Fistulotomy: This surgical procedure involves making an incision along the length of the fistula tract to open it, allowing it to drain and heal properly. In cases where the fistula involves the anal sphincter, a small portion of the muscle may need to be cut. The surgeon’s primary goal is to heal the fistula without compromising sphincter function, as this could lead to complications like bowel incontinence.
- Other Surgical Techniques:
- Seton Placement: A seton is a small rubber or thread-like device threaded through the fistula to keep it open, allowing for continuous drainage and reducing the risk of abscess formation.
- LIFT (Ligation of Intersphincteric Fistula Tract): This technique involves making an incision at the intersphincteric groove, isolating and tying off the fistula tract, removing infected tissue, and suturing the area to promote healing.
- Advancement Flap: A flap is created from nearby tissue (often the rectal wall) to cover the internal opening of the fistula after removing infected tissue. This minimizes cutting the sphincter and helps preserve continence.
- Non-Surgical Options: These include treatments like fibrin glue or collagen plug insertion. Fibrin glue is injected into the fistula tract to seal it and encourage healing, while collagen plugs act as physical barriers. However, these are generally less effective than surgical approaches.
Intersphincteric, Transsphincteric, and Suprasphincteric Fistulas
These are more complex fistulas that often involve varying portions of the anal sphincter, requiring more advanced techniques to minimize complications while promoting healing.
- Fistulotomy: In relatively simple cases, fistulotomy remains a viable option. However, for more complex fistulas, cutting through significant portions of the sphincter muscle is avoided to prevent the risk of bowel incontinence.
- Seton Placement: Setons are often used as a preliminary step to allow for continued drainage and control infection before definitive surgery. They are threaded through the fistula and left in place long-term or temporarily.
- LIFT (Ligation of Intersphincteric Fistula Tract): Ideal for these more complex cases, this procedure involves isolating the fistula tract and sealing it near its internal opening. The infected tissue is removed, and the site is sutured, preventing further infection.
- Endorectal Advancement Flap: This technique involves creating a flap from the rectal wall to cover the fistula’s internal opening after the removal of infected tissue. It’s particularly effective in preserving sphincter function and preventing recurrence.
- Non-Surgical Options: Treatments like fibrin glue or collagen plug insertion are available but often less successful compared to surgical options.
Extrasphincteric Fistulas (the Most Uncommon Type)
These fistulas do not originate in the anal canal and are often the result of trauma, infection, or conditions like Crohn’s disease. Treating extrasphincteric fistulas is highly complex and often requires a combination of approaches.
- Seton Placement: Setons are frequently used to keep the fistula open and draining, either as a long-term solution or in preparation for more invasive surgery.
- LIFT Procedure: Despite its complexity, this technique can sometimes be adapted for extrasphincteric fistulas. It involves isolating and tying off the fistula tract, removing infected tissue, and closing the area with sutures.
- Endorectal Advancement Flap: This procedure is often employed for challenging fistulas like extrasphincteric ones. It aims to close the fistula without cutting sphincter muscles, thereby preserving continence.
- Proctectomy: In severe cases where all other treatments have failed, a proctectomy may be considered. This involves the removal of the rectum and is typically reserved for patients experiencing significant complications or a low quality of life due to the fistula.
Key Considerations for Treatment
The choice of treatment depends on several factors, including:
- The complexity and type of fistula.
- The extent of sphincter involvement.
- The presence of underlying conditions, such as Crohn’s disease.
- The patient’s overall health and lifestyle considerations.
As the condition worsened, I had to return to have a Pezzer drain placed to assist with drainage. Unfortunately, the situation escalated, and I ended up in the emergency room several times with pelvic sepsis. At this point, I was given IV antibiotics. Despite these measures, I was taken to operating room and had another incision and drainage and 2 setons placed a couple of weeks later for a more extensive debridement and the placement of two additional setons. My surgeon believed that surgery was the only option for Fistulizing Perianal Crohn’s until I was irrevocably damaged after surgical mistakes making man-made fistulae’s and then she through her nurse said “Well I’ve done all I can, there are no more surgical Options” Leaving me high and dry to fend or myself with no care team because she told my PCP to back off and not treat my infections she was covering it and was providing all my treatments/Care until her (58 in total) last surgical blunder. THIS CANNOT HAPPEN TO ANOTHER PERSON.





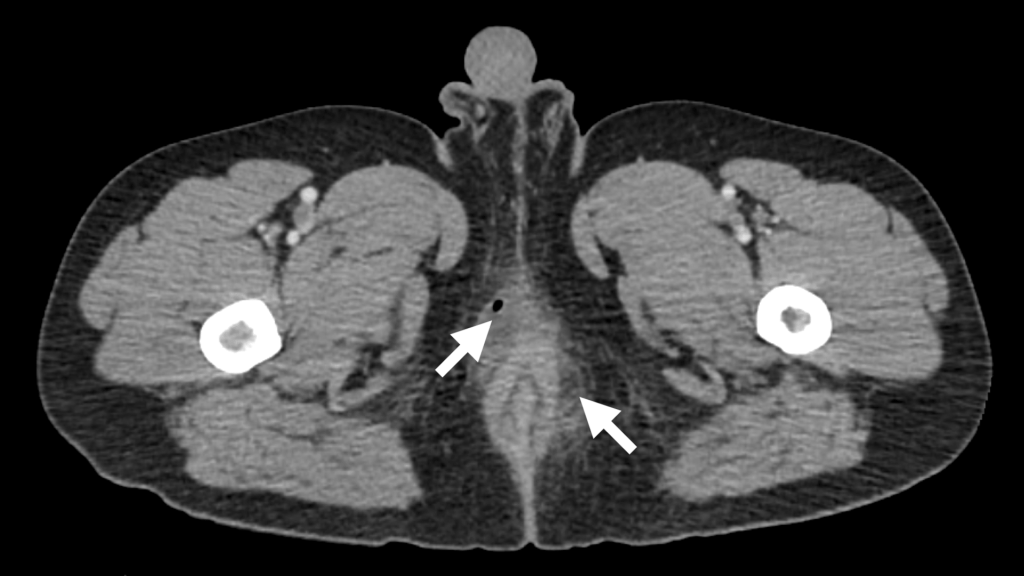
The photos above shows an ischiorectal abscess that initially began as a small almond-sized swelling. Despite my repeated concerns, my doctors ignored the early signs, and the abscess eventually grew to the size of a grapefruit. The first attempt to address it was an in-office incision and drainage procedure, as shown below. However, this failed to fully drain the infection.
For Information about Setons and the aftercare instructions along with some tips and tricks click here
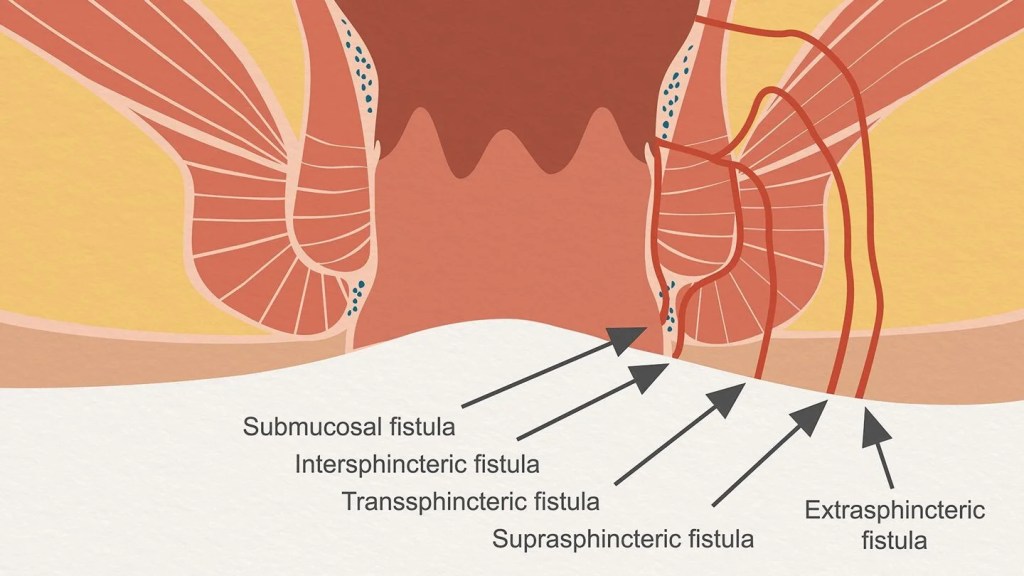
Submucosal Superficial fistula. The track does not involve any Sphincter muscle.
Intersphincteric Track crosses the internal sphincter with a Tract to the perianal skin. It does not involve any External anal sphincter muscle.
Transsphincteric- Tracks from the internal opening at the dentate line via the internal and external anal sphincters, and then it ends in the perianal skin or perineum.
Suprasphincteric Tracks superiorly into the intersphincteric space over the top of the puborectalis muscle, then descends through the iliococcygeus muscle into the ischiorectal fossa and perianal skin.
Extrasphincteric: The track Passes from the perineal skin through the ischiorectal fossa and levator muscles into the rectum. It lies entirely outside the external sphincter complex.
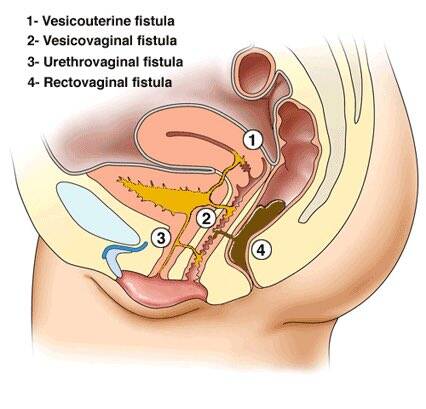
1. VESICOUTERINE FISTULA, is an abnormal connection between the bladder and the uterus.
2. VESIVOVAGINAL FISTULA is an abnormal opening that forms between the bladder and the wall of the vagina.
3. Urethrovaginal – opening between the vagina and urethra, a part of the bladder
4.Rectovaginal – opening between the vagina and rectum/lower part of the large intestine, which carries stool out of the body
- Urethrovaginal – opening between the vagina and urethra, a part of the bladder
- Enterovaginal – opening between the vagina and small intestine
- Colovaginal – opening between the vagina and colon
Treatment Options for Perianal Fistulizing Crohn’s Disease
The treatment of perianal fistulizing Crohn’s disease requires a multifaceted approach, often involving a combination of medical therapies, lifestyle changes, and, when necessary, surgical interventions. This disease is complex and demands collaboration among a multidisciplinary team of specialists, including gastroenterologists, colorectal surgeons, radiologists, and mental health professionals, to achieve the best outcomes.
Antibiotics
Antibiotics are commonly used to manage infections and reduce inflammation associated with fistulas. These medications are particularly effective in addressing secondary infections and alleviating symptoms. Frequently used antibiotics include:
- Metronidazole: A cornerstone treatment for anaerobic bacterial infections and inflammation.
- Ciprofloxacin: Often combined with metronidazole to enhance therapeutic results and reduce infection-related complications.
While antibiotics are an essential part of treatment, they do not address the underlying inflammation caused by Crohn’s disease. Long-term use is not typically recommended due to risks like resistance and side effects.
Biologics
Biologic therapies are highly effective in targeting specific components of the immune system to reduce inflammation, close fistulas, and promote healing. Common biologics include:
- Anti-TNFα Agents:
- Infliximab (Remicade) and Adalimumab (Humira): These biologics are widely used to induce and maintain remission, especially in combination with surgical interventions like seton placement.
- Vedolizumab (Entyvio): A gut-specific integrin antagonist that reduces inflammation by preventing immune cells from reaching inflamed areas in the gastrointestinal tract.
- Ustekinumab (Stelara): Targets interleukins IL-12 and IL-23, addressing inflammation pathways associated with Crohn’s disease.
Combination Therapy
In more complex cases, a combination of antibiotics and biologics may be employed. This approach simultaneously tackles infection and inflammation while promoting fistula healing. However, comprehensive treatment often involves more than just medication.
The Role of Surgery and Multidisciplinary Care
While surgery is a vital tool in managing fistulas, it’s important to remember that it is not the only option. Treating fistulizing perianal Crohn’s disease takes a multidisciplinary approach, with many specialists working together to create a personalized treatment plan. Collaboration between gastroenterologists, colorectal surgeons, radiologists, dietitians, and mental health professionals ensures that all aspects of this complex disease are addressed.
Surgical interventions like setons, fistulotomies, or advancement flaps may be necessary to treat fistulas, but these procedures are often most successful when paired with medical therapy and lifestyle adjustments. Patients should discuss all available options with their healthcare team and seek second opinions when considering invasive procedures.
Mental Health and Advocacy
The emotional toll of perianal fistulizing Crohn’s disease is immense. Chronic pain, frequent surgeries, and unpredictable symptoms often lead to high rates of depression and anxiety. Unfortunately, the mental health challenges associated with this condition are often overlooked.
- Mental Health Support: Working with a therapist or counselor experienced in chronic illness can be life-changing. Mindfulness techniques, support groups, and open communication with loved ones can also help.
- Pain Management: Pain is a significant aspect of this condition, and it’s important to address it with your medical team. Advocating for adequate pain management is essential.
Always remember: you are your best advocate. Trust your instincts, ask questions, and ensure that your voice is heard. Empower yourself with knowledge about your condition and treatment options, as this can significantly improve your quality of life.
Lifestyle Adjustments
- Anti-Inflammatory Diet: Incorporate nutrient-dense foods like fruits, vegetables, lean proteins, and omega-3-rich sources (e.g., salmon and walnuts). Avoid processed foods, refined sugars, and trans fats, as these can exacerbate inflammation.
- Bowel Care to Prevent Constipation: Maintaining bowel regularity is critical, as constipation can increase pressure and worsen symptoms. Staying hydrated, eating fiber-appropriate foods for your condition, and considering stool softeners (if recommended by your doctor) are helpful strategies.
- Quit Smoking: Smoking is a well-established risk factor for Crohn’s disease and its complications, including fistulas. Quitting can reduce inflammation, improve treatment outcomes, and enhance overall health.
The Big Picture
Perianal fistulizing Crohn’s disease is a challenging and complex condition that requires a comprehensive, individualized approach. By combining medical therapies, surgical options (when needed), lifestyle changes, and mental health support, patients can achieve better outcomes and improve their quality of life.
Remember, treatment is not one-size-fits-all. Be proactive, explore every option, and build a trusted healthcare team that truly listens to your needs. For additional guidance, refer to reputable resources like the American Gastroenterological Association or the Toronto Consensus on perianal Crohn’s disease.